Introduction:
Sickle cell disease (SCD) is the most common genetic disease world wide with the highest prevalence in Africa, Middle east, and east Asia. Surgeries in patients with SCD are associated with a higher rate of perioperative complications, however, there is no solid recommendations in the guidelines to advice perioperative transfusion strategies in patients with SCD. This review investigated the current available evidence in the literature to provide a clearer guidance.
Methods:
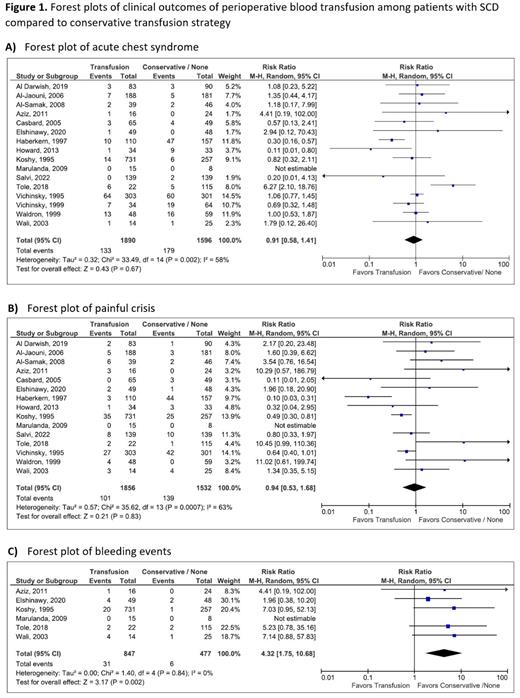
PubMed and Embase electronic search identified 655 articles related to randomized controlled trials and observational studies about the safety of perioperative transfusion in SCD. After removing duplicates and non-relevant articles 39 articles were evaluated in full text for eligibility, of which 24 studies were found eligible for inclusion in qualitative analysis and 16 studies with 3486 participants eligible for inclusion in the quantitative analysis. Assessment of quality and risk of Bias was done using the Cochrane tool for RCTs and ROBBINS-I tool for observational non randomized studies. The safety outcomes of perioperative transfusion, including acute chest syndrome (ACS), painful crisis, neurological complications, fever, minor or major bleeding, thrombosis, intensive care unit (ICU) admission, and all-cause mortality were assessed in comparison to SCD patients undergoing surgeries with conservative transfusion strategy. The risk ratio (RR) with 95% confidence intervals (CI) were calculated for the desired outcomes, the data was combined in forest plots and meta-analysis using the random-effects model.
Results:
Of the 24 studies included, 13 studies had the control arm as no transfusion in comparison to perioperative transfusion, while the remaining studies had conservative strategy guided by hemoglobin level as a control. Sixteen studies reported ACS among SCD patients who received perioperative transfusion (n=1890) versus conservative transfusion strategy (n=1596) (RR= 0.91, 95% CI 0.58-1.41, I2= 58%) (Figure 1-A). Fifteen studies reported painful crisis with perioperative transfusion (n=1856) versus conservative transfusion strategy (n=1532) (RR= 0.94, 95% CI 0.53-1.68, I2= 63%) (Figure 1-B). Neurological complications associated with the perioperative transfusion in SCD (n=1590) compared to conservative transfusion strategy (n=1250) were reported in nine studies (RR= 1.38, 95% CI 0.54-3.57, I2= 0%). Seven studies reported fever as a post-operative complication following perioperative transfusion in SCD (n= 1243) versus conservative transfusion (n= 922) (RR= 1.36, 95% CI 0.94-1.97, I2= 51%). Six studies reported bleeding following perioperative transfusion in SCD (n= 847) versus conservative strategy (n= 477) (RR= 4.32, 95% CI 1.75-10.68, P=0.002, I2= 0%) (Figure 1-C). Three studies reported thrombotic events following the perioperative transfusion in SCD (n= 885) versus conservative transfusion (n= 404) (RR= 0.59, 95% CI 0.06-5.68, I2= 0%). ICU admissions were reported in three studies with perioperative transfusion (n= 53) versus conservative transfusion (n= 147) (RR= 4.99, 95% CI 0.98-25.48, I2= 0%). Mortality was reported in six studies with perioperative transfusion (n= 1320) versus conservative transfusion (n= 977) (RR= 0.67, 95% CI 0.05-8.75, I2= 71%).
Conclusion:
According to this systematic review and meta-analysis Perioperative transfusion in SCD resulted in significantly higher rate of bleeding compare to conservative strategies while the rates of acute chest syndrome, painful crisis, fever, neurological complications, thrombosis, ICU admission, and mortality remained similar between the two strategies.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal